This blog post was first published back in 2013 when there was a lot of attention on breast cancer and the BRCA1 gene mutation, due to Angelina Jolie’s double mastectomy when she didn’t have cancer. I interviewed one of my favorite medical professionals, Dr. C.E. Gant to help dispel some of the myths around this topic and provide you with some truthful information.
Since that time, it has now become common practice for some physicians to recommend mastectomies to women who are healthy if they have the BRCA1 gene mutation. I think this is frightening, appalling, and barbaric. So I’m reposting this discussion during breast cancer awareness month to remind you that you do not have to be a victim to your genes. As you will learn further ahead, there are many steps you can take to protect yourself, and none of them involve cutting off healthy breasts.
Before we get started, let me give you a brief and simplified overview of the BRCA gene mutation for those who may not be familiar with this issue.
BRCA1 is an abbreviation for breast cancer susceptibility gene 1, and BRCA2 is an abbreviation for breast cancer susceptibility gene 2. According to the National Cancer Institute, both are “human genes that belong to a class of genes known as tumor suppressors.” In other words, they help protect the body from cancer. If there is a mutation or defect in one of the genes, then it can’t perform its job and it is believed that this leaves the body more vulnerable to breast and ovarian cancer.
According to the National Cancer Institute, a woman with a BRCA gene mutation is 5 times more likely to develop breast cancer than a woman without a mutation and anywhere between 11 to 36 percent more likely to develop ovarian cancer. Mutations in the BRCA1 gene may also increase a woman’s risk of developing uterine, cervical, colon, and pancreatic cancer, and mutations in the BRCA2 gene may also be associated with an increased risk of stomach, gallbladder, bile duct, and pancreatic cancer, as well as melanoma. Mutations in either gene may also increase a male’s risk of breast, testicular, pancreatic and early-onset prostate cancer, but for males, most cancers are associated with BRCA2 mutations.
However, a very important point you should keep in mind, that is rarely discussed in the media or with patients by their healthcare provider, is that not everyone who has a BRCA gene mutation develops cancer and women who do not have a mutation still develop cancer.
About 12 percent of the general population who does not have a BRCA gene defect develops breast cancer and about 1.4 percent of the general population develops ovarian cancer. Compared to 60 percent for breast cancer and 15 to 40 percent for ovarian cancer in women with a gene mutation.
Another even more important piece of information that the media and medical society is not focusing on, and can also be found at the National Cancer Institute, states that studies on and statistics about the BRCA1 and BRCA2 gene mutations are performed on and calculated from large families with many cancer patients. Since members of a family share not only their genes but environments as well, “it is possible that a large number of cancer cases seen in these families may be due in part to other genetic or environmental factors. Therefore, risk estimates that are based on families with many affected members may not accurately reflect the levels of risk for BRCA1 and BRCA2 mutation carriers in the general population. In addition, no data are available from long-term studies of the general population comparing cancer risk in women who have harmful BRCA1 or BRCA2 mutations with women who do not have such mutations.”
What all of this clearly tells us is that there are other factors that determine whether this gene will express itself or not and it is unclear how much the risk is truly associated with the BRCA gene in and of itself. As I see it, instead of talking about removing body parts to prevent cancer, what we should be looking at is identifying and addressing those factors that influence the gene’s behavior. That is what we will discuss with Dr. Gant.
Dr. C.E. Gant is a practicing physician at National Integrated Health Associates in Washington D.C. and Chief Medical Officer of the Academy of Functional Medicine & Genomics, with more than 30 years of experience in Integrative Medicine, Psychotherapy, and Functional Medicine.
Okay, so here is my interview with Dr. Gant.
Cynthia Perkins:
So, let’s just jump right in Dr. Gant. Is the BRCA gene mutation a death sentence?
Dr. Gant:
No. It is not a death sentence.
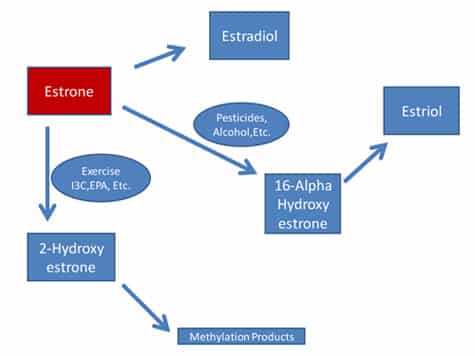
Breast cancer is a multi-causality condition. Genetic vulnerability is just one risk factor. As I read the data, the most important risk factor is whether one of the estrogens called estrone is being metabolized into 2-hydroxyestrone (2-OHE1) or 16-a-hydroxyestrone (16a-OHE1).
Cynthia Perkins:
What is 2-hydroxyestrone and 16-a-hydroxyestrone?
Dr. Gant:
They are metabolites of estrone. You want your estrone to be metabolized into 2-OHE1, which is considered the “good” estrogen, not 16a-OHE1, which is considered the “bad” estrogen. 16-a-hydroxyestrone is associated with an increased risk of breast cancer, lupus and other estrogen related conditions.
Cynthia Perkins:
What determines whether estrone will be converted into 2-hydroxyestrone or 16-a-hydroxyestrone?
Dr. Gant:
The two primary factors are alcohol consumption and pesticides. If someone has a BRCA gene mutation, then the first thing a doctor should do is tell you to avoid alcohol and pesticides. They should also test for the pesticide levels in your body.
Cynthia Perkins:
Are there other factors that cause estrone to be converted into the 16-a-OHE1 form?
Dr. Gant:
Yes, Cimetidine (a medication used to treat ulcers, GERD and heart burn), hypothyroidism, obesity, oral contraceptives, inflammation, oxidative stress, coffee and nicotine.
Cynthia Perkins:
I’ve put together this illustration of estrogen metabolism that I hope will help my blog visitors to understand the conversion of estrone better.
Cynthia Perkins:
Are there other risk factors that a woman should be aware of?
Dr. Gant:
Yes. One should avoid xenoestrogens (man made chemicals that mimic estrogen) of all kinds by consuming organic foods whenever possible, which helps to avoid pesticide exposure.
If nutritional deficiencies are present, then the capacity to clear hormones and toxins from the system can be compromised, so it is crucial to eat a nutrient rich diet and avoid junk foods.
Stress management is important, because when we are under stress, all our nutrients get used up faster and there is an increased need for cortisol. If the demands for cortisol exceed the supply, then the estrogen-inhibiting precursors, most importantly progesterone, which are required to synthesize all sterol hormones will get used up making cortisol and there won’t be enough left over to make other hormones. This is called cortisol steal. Progesterone is important to keep estrogen in balance.
A healthy gut is essential because roughly 70 percent of our immune system resides in and around the intestines, and unhealthy bacteria in the gut can impair one’s ability to get rid of estrogens. It is equally important that the bowels and kidneys be working properly to eliminate estrogens as well.
Hormones are cleared from our system by hooking them to carrier molecules called conjugators, through methylation, glucoronidation and sulfation, so if these detoxification pathways are not working properly, then estrogen can be reabsorbed or not excreted properly, which increases the risk of breast cancer.
Cynthia Perkins:
And what impacts whether the methylation, glucoronidation and sulfation detox pathways are working properly?
Dr. Gant:
Primarily your nutritional intake and exposure to environmental toxins.
Sulfation needs a lot of sulfur based foods like broccoli, cabbage, eggs, and meat or can be increased through supplementation of sulfur based nutrients like methionine and n-acetyl-cysteine. Methylation needs adequate levels of b12, folic acid, b6, magnesium and copper. Glucoronidation can be impaired by unhealthy bacteria in the gut and a product called calcium d-glucarate can assist with this issue. There can also be genetic mutations that impair each of these pathways, and some can be easily identified with genomics testing.
If you are exposed to high levels of environmental toxins on a regular basis, then this can overload and impair the detoxification pathways as well.
Cynthia Perkins:
So what should a woman do to prevent estrone from being converted into 16-a-hydroxyestrone?
Dr. Gant:
Well, first and foremost, she should avoid alcohol, pesticides and herbicides.
Foods that are rich in indole-3-carbinol (I3C, a natural chemical found in cruciferous vegetables like broccoli, cauliflower, cabbage, brussel sprouts and kale and EPA eicosapentaenoic acid (an omega 3 fatty acid) derived from fish and grass-fed beef, both provide powerful prevention against conversion into 16-a-hydroxyestrone and BRCA gene expression. If one is not eating these foods, these nutrients can be consumed in the form of a fish oil supplement and a product called DIM. Soy isoflavones and flax lignans may also upregulate the conversion of 2-hydroxyestrone.
And getting regular exercise is also crucial to upregulate conversion to the 2-hydroxyestone form.
Cynthia Perkins:
Are there any other steps a woman with a BRCA gene mutation should take?
Dr. Gant:
Yes, she should have a hormone health panel performed, which is a simple lab test, to see if she is converting her estrone to 2-OHE1 or 16a-OHE1. This can help one determine their risk of breast cancer far in advance before breast cancer appears, which enables you to make interventions before it begins. Women who are estrogen dominant or anyone concerned about breast cancer risk may want to have this test performed as well.
She should have a thermogram. A thermogram can detect breast cancer roughly five years before a mammogram. It shows congestion of the lymphatics. If there is congestion, then they should do lymphatic drainage, which allows the immune system to see the cancer cells and destroy them. Remember, cancer cells are usually present for a decade or more before the tumors are large enough to find.
And do a breast self-exam more often.
Cynthia Perkins:
How do we know that 16-a-hydroxyestrone is the most important risk factor for breast cancer?
Dr. Gant:
It’s probably not the most important risk factor, but it’s another important one. We are discussing this here in order to demonstrate the risk factor analysis that should be involved in discussions like this, and how risk factors can be modified. Research consistently shows that women with not only breast cancer, but any estrogen sensitive cancer, often have higher levels of 16a-OHE1, than women who do not. Research has also found that making dietary and lifestyle changes, like the ones I suggested above, can decrease levels of 16a-OHE1 and consequently the woman’s risk of developing cancer.
Cynthia Perkins:
Isn’t it true, that cancer is still likely to develop elsewhere, if one is eating a poor diet, drinking alcohol, being exposed to high levels of pesticides and living a life that promotes cancer, regardless of whether the breasts have been removed?
Dr. Gant:
Yes, there is still a far greater likelihood of developing estrogen related cancers, like ovarian and uterine, even if the breast tissue has been removed, if these other risk factors are present, and ovarian cancer is far more serious because it is harder to detect and often progresses to a more advanced, harder-to-treat stage before it is detectable.
It is also possible that breast augmentation itself may increase your risk of cancer, depending on what materials are used. Silicone is also associated with serious autoimmune disease risks.
Cynthia Perkins:
Isn’t it also true that you are at high risk of breast cancer, regardless of whether you have a BRCA gene mutation or not, if you drink alcohol, are exposed to pesticides and herbicides or have any of the other high risk factors going on that push estrone to be converted into the 16-a-hydroxyestrone form?
Dr. Gant:
Yes, because each of these factors upregulate the conversion of estrone into 16-a-hydroxyestrone.
Every woman, not just a woman with a BRCA gene mutation, should prefer that her estrone be converted into 2-OHE1, not 16a-OHE1, and testing for these estrone metabolites which can be done in the standard commercial labs, should be requested. If high levels of 16-a-hydroxyestrone are detected, the shift in genetic expression as discussed here should be done and then the tests should be repeated in a few months, which is usually enough time for the preferable genetic expression to shift.
Cynthia Perkins:
Is the cancer industry engaging in fear mongering which encourages women to engage in radical interventions like preventative mastectomy?
Dr. Gant:
Yes, absolutely. Women are being given a lot of misinformation, disinformation or no information because of certain economic factors. It seems as if empowerment of women to control their own destinies is avoided at all costs. However, there are two sides to the money — greed and fear. For the most part, it is about scaring women for a profit incentive. However, it is also about liability risks when they’re dealing with someone as wealthy as Angelina Jolie. In the case of Angelina Jolie, defensive surgery to protect themselves financially must be recommended.
The wealthier one is, the more likely it becomes that recommendations will be made to protect the providers of healthcare and not the recipient. It is important that the wealthy population understand this.
However, although the cancer industry is complicit in fear-mongering, I believe that oncologists and the rank and file providers of healthcare are unwitting bystanders in the process, forced to comply with certain “standards of care.” Most providers would love nothing more than to provide complete integrative care and healing to the patients they care for, but they dare not in an environment of fear and surveillance.
Cynthia Perkins:
Angelina Jolie was told that she had an 87% chance of developing breast cancer. What are the real chances this gene will express itself?
Dr. Gant:
Well it’s hard to say. We are all treated like rats in a maze as if we were all identical when it comes to determining statistical risk. If one is living in a pesticide laden environment, drinking unfiltered water, not eating organic food and instead eating junk food, drinking alcohol, living a high stress lifestyle and not exercising, then this increases the percentage greatly and the gene is much more likely to express itself under these conditions. Even people without the gene would me more vulnerable if they are engaging in those risk factors. Since most women are living with these risk factors, the statistics are skewed in the direction of much more severe risk than would otherwise be the case.
It also depends on their immune system, whether their liver is congested, if their gut is healthy, if glucoronidation, sulfation and methylation are working and they are getting rid of their estrogens or not.
So, if one modifies their diet and lifestyle to reduce their risk factors, then they can significantly decrease the percentage. So for one person, it may be 87 percent, but for another it may be next to nothing if they are taking fish oil, exercising, have a healthy gut, are avoiding alcohol and pesticides and eating cruciferous vegetables. Remember, a significant percentage of women with the BRCA genes don’t get cancer and the question is rarely asked, what are they doing to avoid it or what are their other protective genetic factors.
This is all true regardless of whether you have the BRCA gene mutation or not; you are going to get breast cancer if you have a lot of these risk factors, with or without a mutation. If you have a BRCA1 or BRCA2 gene mutation, then it will increase the risk substantially.
It’s also worth mentioning the Barbie Doll image that most women in our society are trying to live up to and the impact this has on the immune system. When women can’t live up to this unrealistic expectation of “perfect” breasts which male-expectations and the media imposes with all its conditioning, it promotes disgust and hate towards their body, all of which can weaken the immune system and leave one more vulnerable to cancer. It’s important for women to learn to love themselves just the way they are, as Mr. Rogers once said to all little girls and boys who watched his TV show.
Cynthia Perkins:
Indeed, great point. Anything else you’d like to add?
Dr. Gant:
It’s important for everyone to be aware that terrorism, medical or otherwise, can only work if we are kept in a state of ignorance and helplessness.
The patient is equally responsible for giving in to fear mongering by allowing themselves to be influenced by it and not seeking truthful information.
Cynthia Perkins:
What? Are you saying that the fear mongering behaviors of the cancer industry is an act of terrorism?
Dr. Gant:
Yes, if we define terrorism as, “using terror to achieve one’s economic objectives” then yes, the cancer industry is doing precisely this.
Information, on the other hand, empowers consumers to make better choices and not give in to fear.
Furthermore, fear based people have weak immune systems.
If one does what one can to mitigate risk and then lets go of fear, because life can’t be predicted with absolute certainty anyway, and one lives more in the present, one day at a time, then the immune system becomes stronger and will be more able to destroy cancer cells. This disempowers those who would spread fear and hysteria.
Cynthia Perkins:
Wow, that is powerful Dr. Gant. I have never thought of it in that way. Thank you so much for taking time to talk with me today and sharing your wisdom and truth. It is a pleasure to chat with you again.
Dr. Gant:
My pleasure.
So the primary take away points from my discussion with Dr. Gant are as follows:
It isn’t just the BRCA gene that puts you at risk of breast cancer; it is the combination of many risk factors with estrone conversion being one of the most important. Given the information Dr. Gant has just provided us, a woman with a BRCA gene mutation can significantly reduce her risk of developing breast cancer by simply not drinking alcohol, taking certain supplements and eating better foods, and avoiding exposure to pesticides and herbicides.
Plus, there are a variety of other steps you can take to prevent breast cancer; a double mastectomy is not only unnecessary but may possibly make you even more vulnerable to cancer. As I see it, removing body parts when it isn’t really necessary, is not an empowering and liberating choice. This step should be taken only as a last resort when cancer has already taken over, not as a preventative measure.
Furthermore, all women are at risk of cancer if their estrone is being converted into 16-a-hydroxyestrone instead of 2-hydroxyestrone. However, you have the power to significantly reduce your risk of breast cancer and influence how your genes will express themselves by the foods that you eat and the lifestyle that you live; this is true not only of the BRCA gene but any other gene that is associated with health risks. Last, but not least, every woman has a responsibility to ensure that she is not being manipulated with fear by making sure she is informed and educated truthfully on this topic; this is empowerment.
Although we didn’t touch on the following with Dr. Gant, I would like to add, that the consumption of sugar is a significant risk factor for breast cancer, as sugar feeds cancer cells, and so is a vitamin D deficiency, junk foods of all kinds, insulin resistance, progestins or artificial, non-bio-identical hormones, mammograms and X-rays, petrochemicals, and wearing a bra. I encourage you to read two other articles I’ve written on this topic in the past called, Reduce Your Risk of Breast Cancer and 8 Reasons You Should Burn Your Bra.
Although Dr. Gant would disagree with me on the following issue, it is my opinion that women who are estrogen dominant may have an increase in symptoms from soy and flax. That has been my personal experience, and the experience of many women I work with. Furthermore, soy should only be consumed in a fermented state; anything other than fermented has a variety of negative effects, including cancer. Women who already have cancer may not be good candidates for soy or flax.
Additionally, genistein, a naturally occurring phytoestrogen in soybeans, has been found to increase the estrogenic effects of the herbicide glyphosate, which is commonly known as Roundup. Glyphosate already promotes breast cancer in the parts-per-trillion, but soybeans could increase this risk even further. For these reasons, I do not recommend the consumption of soy.
I leave you with one of my favorite quotes.
“Genes are turned on and off by regulatory genes, and regulatory genes are controlled mainly by nutrients. … there is no drug anywhere that can regulate genetic expression better or more powerfully than diet.”~ Nora T. Gedgaudas, Primal Body Primal Mind
Work with me to make the modifications in your diet and lifestyle that will minimize your risk for breast cancer and encourage optimal health all around. Individualize your diet for your unique biochemical needs, get personalized lifestyle ideas, pinpoint underlying contributors to any conditions you have, and develop a self-care plan to help move you toward a higher level of health.
References
National Cancer Institute – BRCA1 & BRCA2 Cancer Risk and Genetic Testing
https://www.cancer.gov/cancertopics/factsheet/Risk/BRCA
Dr. C.E. Gant
Dr. Bruce Rind – Breast Cancer Webinar
Metametrix Interpretive Guides
https://www.metametrix.com/files/test-menu/interpretive-guides/Estronex-IG.pdf
https://www.metametrix.com/test-menu/profiles/hormones/estronex


Thank you for this EXCELLENT interview and powerful information.