Alzheimer’s is a degenerative brain disease that affects thinking, memory, and behavior which progresses slowly over time and ends with death. It is currently an epidemic in America where it is estimated that approximately 5.4 million people are affected. With a death toll exceeding a half-million Americans each year, it is one of the top three killers in the United States, right on the heels of cancer and heart disease.
Once full-blown Alzheimer’s has set in, there are few if any medical treatments that are effective. However, we are coming to understand many of the causative factors. Like most disease in society today, it is the result of eating the wrong foods, exposure to toxins, and unhealthy lifestyle choices, which means you can take a variety of steps to protect your brain and decrease your risk. Let’s explore these risk factors by answering the following question from a site visitor.
Hi Cynthia,
Is it true that Alzheimer’s is actually Type 3 Diabetes? That Alzheimer’s, Dementia, and other types of Mental Conditions are all tied to sugar consumption? ~Jayson
Hi Jayson,
Before I answer that question, let’s take a quick look at what’s going on in the brain with Alzheimer’s so that the rest of what I’m going to present will make sense.
Alzheimer’s is only one form of dementia, but it is the most common and severe. The first signs of dementia typically present as forgetfulness. There may be changes in personality or emotional behavior, memory, language, perception, thinking, and judgement. Then mild cognitive impairment may appear with difficulties in problem-solving, performing more than one task at a time, taking longer to perform those tasks, and recalling recent conversations or events. People with mild cognitive impairment are usually aware of these changes and they do not significantly impair their day-to-day activities. Mild cognitive impairment does not always advance to Alzheimer’s, but when it does, then symptoms become more obvious and disruptive.
At this point, which is then considered the early stages of Alzheimer’s there is difficulty in carrying out more tasks, particularly those that require a considerable amount of thought like balancing the checkbook or playing games, as well as learning new information and routines. They may get lost on routes that are familiar to them and have an inability to retrace their steps, have problems with word find, misplace things, lose interest in activities they used to enjoy, experience dull or depressed mood, a decrease in social skills, and changes in personality.
As Alzheimer’s progresses, then it begins to impair their ability to take care of themselves with a decreased inability to prepare meals, dress properly, drive, read, and write. Forgetfulness is now expanded to their own life history and who they are, and they may experience agitation, disrupted sleep patterns, poor judgment, inability to recognize danger, depression, hallucinations, delusions, become argumentative or even violent, and withdrawal from social contact. In language, they don’t use the right words or know how to pronounce them accurately and sentences may not make sense.
In the advanced stage of Alzheimer’s, the individual can no longer recognize family members, understand language, or perform basic daily activities like eating, bathing, and getting dressed. They may also experience incontinence and difficulty swallowing.
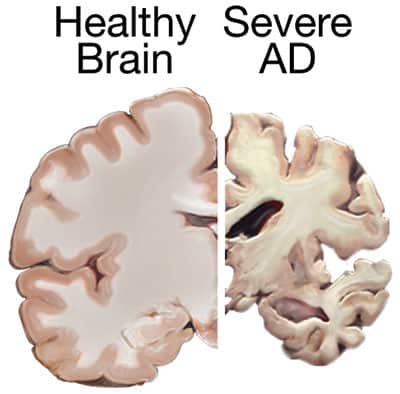
When we look at the brain of someone with Alzheimer’s, we see the following characteristics that are not exhibited in healthy brains:
- Neurons (brain cells) that have developed neurofibrillary tangles, which are fragments of protein that are twisted up and clog the cell. Nutrients can no longer travel through the cell and they die. The primary element of a tangle is a protein called tau.
- Neuritic plaques, which are abnormal clusters of brain cells, protein, and nerve cells that are dead or dying.
- Senile plaques which are areas where dead or dying nerve cells accumulate around protein.
- Much fewer brain cells and synapses (connections with other neurons) than healthy brains.
- Ventricles, which are spots in the brain filled with fluid, are larger.
- Significant shrinkage in the size of the brain due to widespread cell death. Shrinkage is most severe in the hippocampus, which is our memory center.
These plaques are referred to as amyloid plaques which are formed from a toxic protein-peptide called beta-amyloid. Some people without Alzheimer’s may develop plaques as they age as well, but the brain of an Alzheimer’s patient has much more in certain areas. It is unknown whether plaques and tangles cause Alzheimer’s or if they are a byproduct of the process that is taking place. Both plaques and tangles were discovered by Dr. Alois Alzheimer’s, thus the name of the condition.
In the book Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar–Your Brain’s Silent Killers by Dr. David Perlmutter (a book that everyone should read) he explains that plaques are a “build-up of an odd protein that essentially hijacks the brain and takes the place of normal brain cells.”
The rate of progression can vary greatly from individual to individual and the plaques and tangles tend to spread more widely throughout the brain as Alzheimer’s progresses. On average, they will live about eight years after a diagnosis, but some may live up to 20, depending on when the diagnosis is made and whether the individual has other health conditions as well. Occasionally, Alzheimer’s comes on quickly, and when that is the case, progression is typically faster.
So the goal in preventing Alzheimer’s is to identify what is happening that causes these changes in the brain to occur.
Sugar, Inflammation and the Brain
There is significant research that suggests that one of the primary causative factors for Alzheimer’s and other dementias may be the presence of sugar in the diet. And we aren’t just talking about table sugar or high-fructose corn syrup. Whole grains, fruit, potatoes, and any other high starch food that breaks down into sugar contribute as well. As a matter of fact, whole grains increase blood sugar more than sugar itself.
When we eat sugar or carbohydrates of any kind, it causes our blood sugar levels (glucose) to rise rapidly, which signals the pancreas to release insulin to bring the blood sugar levels back down. If the diet is consistently high in sugar or carbohydrates, insulin will be released on a frequent basis, and eventually, glucose receptors become less responsive or desensitized to insulin, which is called insulin resistance.
Insulin resistance prevents glucose from being carried into the cell for energy or being stored as glycogen or fat, and instead it remains in the bloodstream, keeping blood sugar levels abnormally high. The higher the level of glucose in the bloodstream, the more insulin is being released. The more insulin is being released the more resistant the receptors become. The more resistant they become the more insulin is released. If this cycle continues, eventually the pancreas get wore out and receptors stop responding to insulin at all and type 2 diabetes occurs.
So what does all this have to do with Alzheimer’s? Well, according to Dr. David Perlmutter, insulin resistance “sparks the formation of those infamous plaques that are present in diseased brains like Alzheimer’s.”
High levels of insulin trigger high levels of inflammation, and we are beginning to discover that inflammation is at the core of all degenerative health conditions including brain disorders or diseases. Inflammation is the body’s normal response to some type of stress in the body. If it believes we are facing something potentially dangerous, it defends itself by releasing a variety of chemicals that produce the side-effect of pain and swelling; the telltale sign of the inflammatory process.
Inflammation is critical for our survival because it protects us from harm. It’s what helps us heal when we cut ourselves or are bitten by an insect, protects us from microbial invasion, and attacks viruses or bacteria that manage to invade. However, it is supposed to be short-lived, because these chemicals are toxic to our cells. “It leads to a reduction of cellular function followed by cellular destruction.” If the inflammatory process gets out of control and we remain in a constant state of inflammation, it spreads to other parts of the body. We are now coming to understand that this inflammation is a root contributor to heart disease, cancer, arthritis, type 2 diabetes, obesity, and much more.
What most people don’t realize is that this inflammation is also reaching the brain and is a major driving force behind neurological disorders like Alzheimer’s. Cytokines, the cellular mediators of inflammation, have been found to be dramatically elevated in individuals with degenerative brain disorders like Alzheimer’s, Parkinson’s, MS, and autism. Dr. Perlmutter explains that “cytokines are highly antagonistic to the brain, damaging tissues and leaving the brain vulnerable to dysfunction and disease – especially if it continues.” A diet that is high in carbs is one of the predominant stimulators for inflammation that reaches the brain.
Inflammation in the brain turns on a chemical pathway that increases the production of free radicals, this process is known as oxidative stress. Oxidative stress is also a normal and necessary part of life, but it if it runs out of control it is lethal. Normally electrons occur in pairs, but a variety of factors like poor diet, stress, toxins, pollution, and normal processes in the body like when we burn food for energy, can free one of the electrons from a molecule. This freed electron (free radical) then becomes rogue and runs around trying to steal electrons from other molecules. This process incites more inflammation. “Oxidized cells and tissues don’t function normally,” which leaves the individual vulnerable to many degenerative health conditions.” High levels of free radicals also weaken the immune system.
Antioxidants, (A, C, E, Coq10) are used to reduce oxidation, which also reduces inflammation because they donate an electron to the free radical, which interrupts the process and helps prevent damage. However, most people are not eating the foods that are rich in antioxidants like plants, berries, nuts, and meat, so they aren’t getting adequate antioxidants to even manage the amount of oxidative stress that occurs with normal body processes.
The key take away here is high oxidation = high inflammation.
Unlike the rest of the body, the brain has no pain receptors. Therefore, we are not aware that inflammation is happening in the brain until it is already too late. Once Alzheimer’s presents, the damage is already so severe that is very difficult to turn around.
Inflammation in the brain is not only associated with Alzheimer’s but MS, Parkinson’s, autism, depression, epilepsy, Tourette’s, attention deficit, anxiety disorders, schizophrenia, headaches, and any other mental health or neurological disorders.
Blood Sugar and Brain Shrinkage
Furthermore, high blood sugar (which is caused by eating carbohydrates, even the complex ones) is also associated with brain shrinkage. Even individuals who have blood glucose levels that are on the high end of normal (90 to 100) are at a much greater risk of brain shrinkage. This indicates that the standards set by our medical society need to be redefined and if you want to prevent brain shrinkage, then your blood glucose levels need to be lower than what is generally considered to be normal.
Even slightly elevated blood sugar is correlated directly with a greater risk for shrinkage of the hippocampus, our memory center, and a distinctive feature of Alzheimer’s. Elevation of hemoglobin A1c, which provides an average for blood sugar over a three to four-month period, is also correlated with an increase in brain shrinkage.
So, it is for these reasons that many health care providers are beginning to call Alzheimer’s a type 3 diabetes. Sugar, grains, and other high carb foods destroy the brain and result in not only dementia and Alzheimer’s, but ADHD, depression, Tourette’s, autism, anxiety disorders, epilepsy, compulsive overeating, addiction, violence, aggression, antisocial behavior, and many other mental health or neurological disorders as well. However, even though it is very clear that sugar and glucose levels play a significant role in dementia or Alzheimer’s, it is vital to be aware that this is only “one” of many causative factors.
In my opinion, it is not completely accurate to label Alzheimer’s “solely” as a type 3 diabetes condition, because that then closes the door and the mind to looking at what else may be contributing. Yes, indeed sugar and carbs are one of the primary issues, and in some cases, it may be the only issue, but other factors we will discuss below that have a clear correlation must not be ignored.
Cholesterol and Alzheimer’s
For example, it’s not only the consumption of the wrong foods that can lead to degenerative brain disorders but equally important is the food that is often missing from the diet like cholesterol. Cholesterol is vital for normal and healthy brain function because it assists in neuron function, serves as a fuel for neurons, and is a basic building block in the cell membrane itself. It also serves as an antioxidant and interacts with sunshine to produce vitamin D, which is another brain critical nutrient that plays a vital role in inflammation and immune function.
Vitamin D aids in controlling enzymes in the brain and cerebrospinal fluid that are concerned with constructing neurotransmitters and activating nerve growth. It also shields neurons from the harmful effects of free radicals and lessens inflammation.
Numerous studies indicate that individuals with insufficient vitamin D levels experience significantly more decline in cognitive functioning than those with higher levels. One study found that subjects with the highest intake of vitamin D had a 77 percent decrease in risk for Alzheimer’s. Vitamin D can also produce antimicrobial peptides that defend the body against yeast, viruses, and bacteria, which could potentially trigger more inflammation.
The brain acquires cholesterol through the bloodstream via LDL. According to Dr. Perlmutter, “sugar molecules attach themselves to LDL” and change its shape, which renders it less useful and increases free radicals, and becomes incapable of delivering cholesterol to the neurons. This is just one of the important roles of LDL. It is oxidized LDL that causes heart disease, not LDL. Vitamin D can also be acquired to some extent through cold water fish and mushrooms.
In the infamous Framingham study that has been ongoing since 1948, it demonstrates that when cholesterol is low that brain function declines. Individuals who had cholesterol levels below 200, which is what medical authorities say we should strive for, performed worse in areas of abstract reasoning, attention, concentration, word fluency, and executive functioning, than those with borderline high or high levels of cholesterol. People with the highest cholesterol scored best. This means that if you’re taking statins to lower your LDL, then you are increasing your risk for heart disease and decline in cognitive function, not to mention the inability to make cortisol and all your other steroid hormones since cholesterol is also the precursor to them.
Mad Cow and Alzheimer’s
A recent study has suggested that an infectious protein called TDP-43, which is the protein responsible for Mad Cow Disease and Chronic Wasting Disease in deer and elk, and maybe implicated in ALS disease, may also be a major player in the development of Alzheimer’s and other dementia, because it is correlated with shrinking of the hippocampus, which results in memory loss.
In this study, they performed an autopsy on the brains of more than 340 individuals with Alzheimer’s and discovered that TDP-43 was present in about 200. What’s really interesting about this study is that they examined the brains of two different groups of people with Alzheimer’s; those who exhibited symptoms and those that didn’t. The patients that had TDP-43 were 10 times more likely to be exhibiting symptoms at death than those without the protein.
This is very important because it demonstrates that many people who have the beta-amyloid plaques and tangles in the brain that are believed to cause Alzheimer’s, don’t always exhibit symptoms of Alzheimer’s.
Therefore, this suggests that there is some other contributing factor that determines whether amyloid plaques and tangles actually produces Alzheimer’s. It may be that when it is combined with some other factor like TDP-43 or other factors not yet known.
To complicate things further, another study at the University of Pennsylvania found that TDP-43 reacts to oxidative stress, suggesting that TDP-43 may become lethal when some other factor like oxidative stress is present, which fits in with the oxidative stress factors that we discussed earlier.
Mad Cow is caused by feeding cattle animal by-products, which is a common practice in confined animal feeding operations (CAFOs). Additionally, there are other foreign proteins besides TDP-43 that are present in CAFO raised animals. Any foreign protein in the body incites inflammation, and as we mentioned, inflammation is correlated with numerous degenerative diseases. And, CAFO animals are also fed feed that is loaded with genetically modified grains, which also generate foreign proteins, that will result in inflammation.
In cattle, the incubation period for Mad Cow Disease is about five years, but it may be as long as ten years before symptoms manifest in humans. It slowly eats holes in the brain, eventually making it sponge-like and ultimately resulting in death. Very similar to Alzheimer’s.
Therefore, it would seem that if one wants to prevent Alzheimer’s or other dementias, as well as numerous other health problems, they would avoid eating meat raised in CAFOs and eat organic free-range, grass-fed meat instead.
Lower Levels of BDNF
Studies have also demonstrated that individuals with Alzheimer’s have decreased levels of BDNF (brain-derived neurotrophic factor.) A gene located on chromosome 11 “codes for the production of this substance,” which “plays a key role in neurogenesis” the creation of new neurons. It also “protects existing neurons and ensures the survival of neurons by encouraging synapse formation.”
Low levels of BDNF are also found in individuals with depression, schizophrenia, OCD, and other mental health issues. When the BDNF pathway is activated, it also increases the efficacy of your detoxification system, which can also benefit dementia, since it will eliminate many of the toxins associated with brain disorders.
Higher levels of BDNF are also associated with a decrease in appetite.
DHA (Docosahexaenoic Acid)
The brain is two-thirds fat and one-quarter of that is DHA, which is a very important omega-3 that provides building blocks for the membranes that surround brain cells, especially the synapses, and the activation of BDNF.
It also helps regulate inflammation by reducing the activity of the COX-2 enzyme, which incites the manufacturing of the chemicals that inflict damage on the cells. Dr. Perlmutter states that DHA “helps orchestrate the production, connectivity and viability of brain cells, while at the same time enhance function.”
Aluminum in the Brain of Alzheimer’s
High levels of aluminum are commonly found in the brains of individuals with Alzheimer’s. Dr. Joseph Mercola explains that “aluminum is to your central nervous system, as cigarette smoke is to your lungs.” Aluminum, like all toxic metals, “damage brain tissue and produce oxidative stress,” which means high levels of inflammation. Aluminum also impedes your ability to produce glutathione, a vital substance needed for detoxification and managing oxidative stress.
Aluminum can be found in cookware, baking powder, prescriptions, vaccines, toothpaste, antiperspirants, some brands of nutritional supplements, and food.
Other heavy metals like cadmium, mercury, arsenic, lead, and copper are also neurotoxic, and may produce numerous deficits in cognitive functioning.
Gluten and the Alzheimer’s Brain
The protein in gluten (glutenins and gliadin) also prompt inflammation and we’re not just referring to celiac disease. Celiac disease is the most extreme form of gluten sensitivity, but we are all sensitive to gluten on some level. Our bodies produce a substance called zonulin when we consume gluten, which makes the gut more permeable (leaky gut). This allows proteins to get into the bloodstream that shouldn’t be there. The immune system sees this protein as a foreign invader and launches an attack, which incites inflammation not only in the gut, but the brain as well. Zonulin is also an important component of the blood-brain barrier, high levels can cause destruction of the barrier and result in leaky brain, whereby the barrier allows substances to cross over into the brain that shouldn’t be there.
An individual with gluten sensitivity may not experience any gastrointestinal symptoms; instead, it may manifest purely in the brain with a wide variety of symptoms like dementia, schizophrenia, OCD, ADHD, depression, psychosis, autism, and more.
Additionally, antibodies that are created against gliadin, can “directly combine with specific proteins found in the brain that look like gliadin protein, which leads to the formation of more inflammatory cytokines.”
However, gut permeability is also increased by other factors like Candida overgrowth, H pylori and other bacteria, SIBO, parasites, legumes, phytates, alcohol, chlorinated water, caffeine, artificial sweeteners, pesticides like Roundup, antacids, and a variety of pharmaceuticals.
Although gluten is the most common food to cause inflammation, casein in dairy is another frequent offender. As mentioned previously, the body responds to any foreign protein in the body with an immune response and the inevitable inflammation; therefore, sensitivity to any food can participate in this process and contribute to inflammation.
Pesticides, Herbicides, and Other Toxins
Several studies have indicated that individuals exposed to pesticides and herbicides of many different kinds have a greater risk of developing dementia and Alzheimer’s later in life, which really should come as no surprise since pesticides and herbicides are known neurotoxins (target the brain and nervous system.)
One study suggests that the pesticide DDT may increase not only the risk of developing Alzheimer’s, but the severity of the condition as well. It appears to increase the proteins that are associated with the formation of plaques found in the brain of Alzheimer’s. Individuals with the highest level of DDE (the compound that is left when DDT is broken down) had the most severe cognitive impairments. Levels of DDE were four times higher in the subjects with Alzheimer’s than the control group.
Although DDT was banned in the United States in 1972, it continues to be used heavily in other countries. Therefore, if you are consuming food products that have been imported or fish from waterways that may be contaminated, you are still being exposed. It takes decades for DDT to break down, therefore Americans are still being exposed to it directly in this country. According to the Centers for Disease Control and Prevention, DDT is still found in 75 to 80 percent of blood samples collected.
Numerous studies have demonstrated a correlation between pesticides and herbicides like Roundup with other severe neurological disorders like Parkinson’s, depression, and autism. One study found that your risk for Parkinson’s is increased by 75 percent when exposed to a pesticide called Maneb. It is safe to assume they would be just as likely to contribute to Alzheimer’s. Pesticides of many different kinds have been shown to damage the brain in numerous ways.
Toxins of all kinds that are found in your common every day life and products like air pollution, water, cosmetics, household cleaning supplies, perfumes, colognes, air fresheners, and personal care products can also prompt an immune response and inflammation, thus possibly contribute to dementia and Alzheimer’s.
Furthermore, in order for the body to detoxify toxins, it creates oxidative stress. The more toxins you are exposed to, the more oxidative stress being generated. As we discussed earlier, high levels of oxidative stress result in high levels of inflammation, which can be experienced in the brain.
It’s also important to note that Candida overgrowth, lyme, SIBO or other types of bacterial infections, parasites or any type of microbial infection release numerous toxins that the body must detoxify, which means they also contribute to oxidative stress and inflammation.
Additionally, toxins can also change “how our genes express themselves, and fire of the autoimmune response,” or inhibit BDNF.”
Lack of Exercise
Studies have demonstrated that exercise can actually increase the size of the brain’s memory center, while individuals who don’t exercise have brain shrinkage. It also helps neurons be more nimble and capable of multitasking and activates BDNF, which means it helps form new neurons and build new neuronal networks.
Exercise also improves insulin sensitivity, thereby lowering glucose levels, demonstrated by the fact that hemoglobin A1c is lower in individuals who exercise.
It is also a powerful anti-inflammatory; activating the Nrf2 pathway, which turns on genes that suppress inflammation. Nrf2 is a pathway that is activated automatically when free radicals are high, which enables the body to produce antioxidants and improve detoxification. Nrf2 can also be activated with calorie restriction, DHA, curcumin, silymarin, and sulforaphane that is present in broccoli.
C-reactive protein, a marker for how much inflammation is in the body, is lower in people who exercise. However, be sure to note that exercise should be mild and gentle. Too much exercise is just as harmful as not enough.
How to Reduce Your Risk for Alzheimer’s
As we can see, there are many risk factors that may contribute to the development of dementia and Alzheimer’s. Although it is distinctly possible to be a type 3 diabetes to a large degree, it is most likely the combination of all these factors together, which when combined creates a perfect storm.
The majority of individuals with Alzheimer’s have been eating wheat, casein, GMOs, CAFOs, and a high carbohydrate diet, and being exposed to numerous toxins, dealing with high levels of oxidative stress and inflammation, and not consuming enough fat or cholesterol on a day-to-day basis. Therefore, they have all the risk factors.
The good news is that you can reduce your risk for developing Alzheimer’s by reducing oxidative stress and inflammation, lowering your glucose levels, increasing your fat and cholesterol intake, avoiding exposure to pesticides, herbicides, and other environmental toxins, encouraging a healthy gut, and turning on the gene pathway that activates BDNF and Nrf2.
All of this can be achieved by eating an organic, low-carb, Paleo diet (ketogenic diet), consuming more foods with DHA like salmon, getting regular, but mild exercise, living an environmentally friendly lifestyle, avoiding gluten, casein, GMOs, and CAFO meat, getting adequate sleep and exposure to sunshine, eating more foods that are rich in fat and cholesterol, and possibly supplementing with curcumin.
A ketogenic diet alone activates BDNF, protects brain cells from toxins, improves the detoxification system, increases antioxidants, decreases oxidative stress and free radical production, prevents cell dell, increases growth of new mitochondria, lowers blood glucose levels, creates new neurons, strengthens and protects the neuronal network, and reduces amyloid in the brain (the protein that is present in brain plaque), increases efficacy of metabolism, encourages GABA production and lowers glutamate. So clearly, like all other health matters, the food you eat is the most important component for a healthy brain.
If you need help overcoming your cravings so that you can remain committed to a low-carb diet and protect yourself from insulin resistance, type 2 diabetes, dementia, and Alzheimer’s, check out my toolkit, which provides everything you need to break free from sugar and carbs with ease.
References
Dr.David Perlmutter, Grain Brain: The Surprising Truth About Wheat, Carbs, and Sugar – Your Brain’s Silent Killers. Little, Brown and Company; 1st edition 2013.
Dr. Joseph Mercola, Study: The Alzheimer’s – Aluminum Direct Link
<https://articles.mercola.com/sites/articles/archive/2014/03/22/aluminum-toxicity-alzheimers.aspx?>
A.D.A.M. Medical Encyclopedia. PubMed Health. Alzheimer’s disease. Senile dementia – Alzheimer’s type (SDAT); SDAT Last reviewed: September 26, 2011. <www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001767/>
Dr. Charles Gant. Academy of Functional Medicine & Genomics. Detoxification Modules.
Dr. Joseph Mercola. The Alzheimer’s Mad Cow, and Chronic Wasting Disease Connection <https://articles.mercola.com/sites/articles/archive/2014/07/31/alzheimers-mad-cow-chronic-wasting-disease.aspx>
Rutgers Biomedical and Health Sciences. “DDT pesticide exposure linked to Alzheimer’s disease, study shows.” ScienceDaily. ScienceDaily, 27 January 2014. <www.sciencedaily.com/releases/2014/01/140127164406.htm>.
Tyas SL, Manfreda J, Strain LA, Montgomery PR. Risk factors for Alzheimer’s disease: a population-based, longitudinal study in Manitoba, Canada.Int J Epidemiol. 2001 Jun;30(3):590-7. <www.ncbi.nlm.nih.gov/pubmed/11416089>
Nature Reviews Neurology 6, 353 (July 2010) | doi:10.1038/nrneurol.2010.80 <https://www.nature.com/nrneurol/journal/v6/n7/full/nrneurol.2010.80.html>
K.M. Hayden, PhD, M.C. Norton, PhD, D. Darcey, et. al. Occupation exposure to pesticides increases the risk of incident AD. Neurology May 11, 2010 vol. 74 no. 19 1524-1530 <www.neurology.org/content/74/19/1524.abstract>
Brain image courtesy of the National Institute on Aging/National Institutes of Health.